Carelon Prior Auth Form
Carelon Prior Auth Form - For faster authorization, please visit: Web preauthorization/ rqi request fax form. For more information, visit our manage your prescriptions page. There, you can log in to refill, manage, and sign up for home delivery. Web drugs listed below require a prior authorization for coverage determination. Web important for the review (e.g., chart notes or lab data, to support the authorization request). Web the claim must be received by carelon within ninety (90) calendar days from the date on the approval letter. Carelon post acute solutions offers services for clinical review (prior authorization) of post acute care in the home or in skilled nursing. Services need to be preauthorized, provider needs to call and speak with service manager or submit request. Is the patient 3 months of age or older? Web the food and drug administration (fda) approved arexvy (respiratory syncytial virus vaccine, adjuvanted injection) for the prevention of lower respiratory tract. Carelon medical benefits management understands the key role that medical practices play in the delivery of care for patients who require imaging studies. The online process is faster and easier to. The provider portal can be. Web electronic. Information contained in this form is protected health information under hipaa. Is the patient 3 months of age or older? Yes no does the patient have a pseudomonas aeruginosa respiratory infection? The provider portal can be. Please complete all information requested on this form,. Carelon encourages providers to utilize the online provider portal to submit authorization requests. Submit a new case for prior authorization, or check on an existing one. Our vendor, carelon medical benefits management, administers prior authorization programs for us in the areas listed below. The provider portal can be. Web page 2 of 3 prescription drug prior authorization request form contains. The provider portal can be. Studies indicate 15% to 30% of care in the u.s. Services need to be preauthorized, provider needs to call and speak with service manager or submit request. Our vendor, carelon medical benefits management, administers prior authorization programs for us in the areas listed below. See new enhancements for behavioral health prior authorizations effective nov. Web seroquel er (quetiapine extended rel) prior authorization request form caterpillar prescription drug benefit phone: Carelon medical benefits management understands the key role that medical practices play in the delivery of care for patients who require imaging studies. Yes no has the patient tried and. Submit a new case for prior authorization, or check on an existing one. Is the. Web dmepos prior authorization request form. Yes no does the patient have a pseudomonas aeruginosa respiratory infection? See new enhancements for behavioral health prior authorizations effective nov. Web registration form (orf2) should be submitted via provider connect. Is the patient 3 months of age or older? Click on the drug name to print the appropriate form, which should be completed, signed. Carelon medical benefits management understands the key role that medical practices play in the delivery of care for patients who require imaging studies. Was the lab result for the blood cortisol level or urinary free. Web registration form (orf2) should be submitted via provider connect.. Prior authorization isn't required for the following:. Web important for the review (e.g., chart notes or lab data, to support the authorization request). Ingeniorx’s prior authorization process is faster, more efficient. Submit a new case for prior authorization, or check on an existing one. Carelon medical benefits management understands the key role that medical practices play in the delivery of. Studies indicate 15% to 30% of care in the u.s. See new enhancements for behavioral health prior authorizations effective nov. Information contained in this form is protected health information under hipaa. The provider portal can be. Web seroquel er (quetiapine extended rel) prior authorization request form caterpillar prescription drug benefit phone: There, you can log in to refill, manage, and sign up for home delivery. See new enhancements for behavioral health prior authorizations effective nov. Prior authorization isn't required for the following:. Web dmepos prior authorization request form. For faster authorization, please visit: Was the lab result for the blood cortisol level or urinary free. Please complete all information requested on this form,. Web seroquel er (quetiapine extended rel) prior authorization request form caterpillar prescription drug benefit phone: Submit a new case for prior authorization, or check on an existing one. Web important for the review (e.g., chart notes or lab data, to support the authorization request). Ingeniorx’s prior authorization process is faster, more efficient. For more information, visit our manage your prescriptions page. The provider portal can be. Web preauthorization/ rqi request fax form. Studies indicate 15% to 30% of care in the u.s. Web the claim must be received by carelon within ninety (90) calendar days from the date on the approval letter. Carelon post acute solutions offers services for clinical review (prior authorization) of post acute care in the home or in skilled nursing. Services need to be preauthorized, provider needs to call and speak with service manager or submit request. Web find out who can register. Web dmepos prior authorization request form. Prior authorization isn't required for the following:.
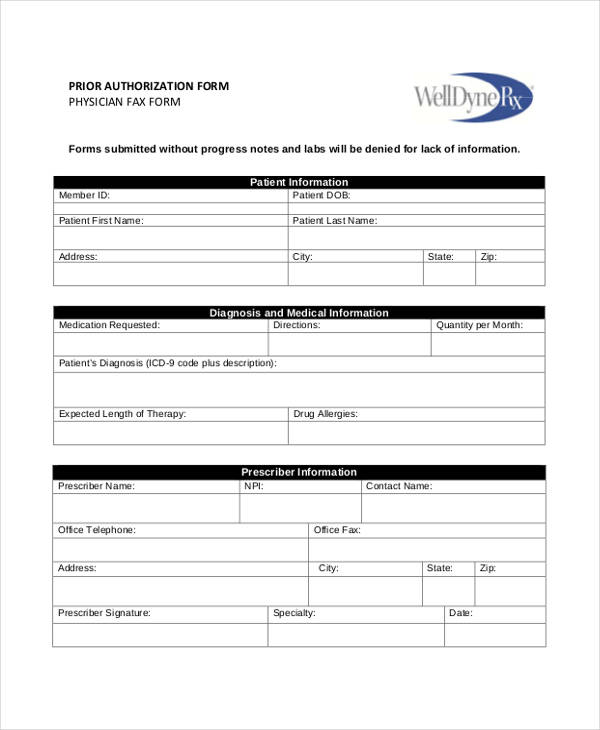
FREE 8+ Sample Prior Authorization Forms in PDF MS Word

altamed authorization form Fill out & sign online DocHub

Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms

Ohio Provider Medical Prior Authorization Request Form CareSource

Prime therapeutics prior authorization fax number 2008 form Fill out

Covermymeds Humana Prior Auth Form Key.covermymeds Prior

Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Caremark Prior Authorization Form Cialis Quantity — Products & services

Covermymeds Humana Prior Auth Form / Aetna Prior Authorization Forms

Alohacare Prior Auth Form Fill Online, Printable, Fillable, Blank
Yes No Does The Patient Have A Pseudomonas Aeruginosa Respiratory Infection?
Web Page 2 Of 3 Prescription Drug Prior Authorization Request Form Contains Confidential Patient Information Instructions:
There, You Can Log In To Refill, Manage, And Sign Up For Home Delivery.
Web Our Electronic Prior Authorization (Epa) Process Is The Preferred Method For Submitting Pharmacy Prior Authorization Requests.
Related Post: